What Is Diastais Recti And Do You Need To Be Concerned?
Have you watched the movie “The Waterboy” with Adam Sandler? It’s one ridiculous piece of cinematic history simply because it’s so out there. And it goes to show you how far we’ve come in social acceptance. A movie like that, wouldn’t fly with most people today.
Every time I see a discussion or post on social media regarding abdominal separation, I’m reminded of Helen, the Waterboy’s mom who calls pretty much everything she doesn’t understand “the devil” and What I hear when there’s a fitness or rehab product promising to heal abdominal separation is “Diastasis Recti is the devil”
And I believed this at one point myself. Probably even looked like Kathy Bates as I said it. I love Kathy Bates by the way.
Diastasis Recti is not the devil
Research has come a long way when it comes to abdominal separation (aka diastasis recti). When I first started learning about this natural occurrence during pregnancy, abdominal separation was far from ideal if it remained past 8 weeks postpartum.
Unfortunately, women are still running scared when it comes to abdominal separation. I see it in my clients and online. I myself had a separation following my second pregnancy and felt a little on the broken side. Throw a prolapse in there as well and I was a giant body of mess.
Until recently, if you noticed coming or coming in your belly, you were told to avoid certain movements like:
- Crunching
- Twisting
- Overhead movements like pressing and pulling
- Planks
Because…these movements–”the devil” Just kidding.
For some women with DR, it may be recommended they retrain these movements because they can’t maintain tension, but this is temporary. As your body becomes stronger, your core will become better capable to handle the work you’re trying to place on it. Think, progressive overload.
What is abdominal separation (DR)?
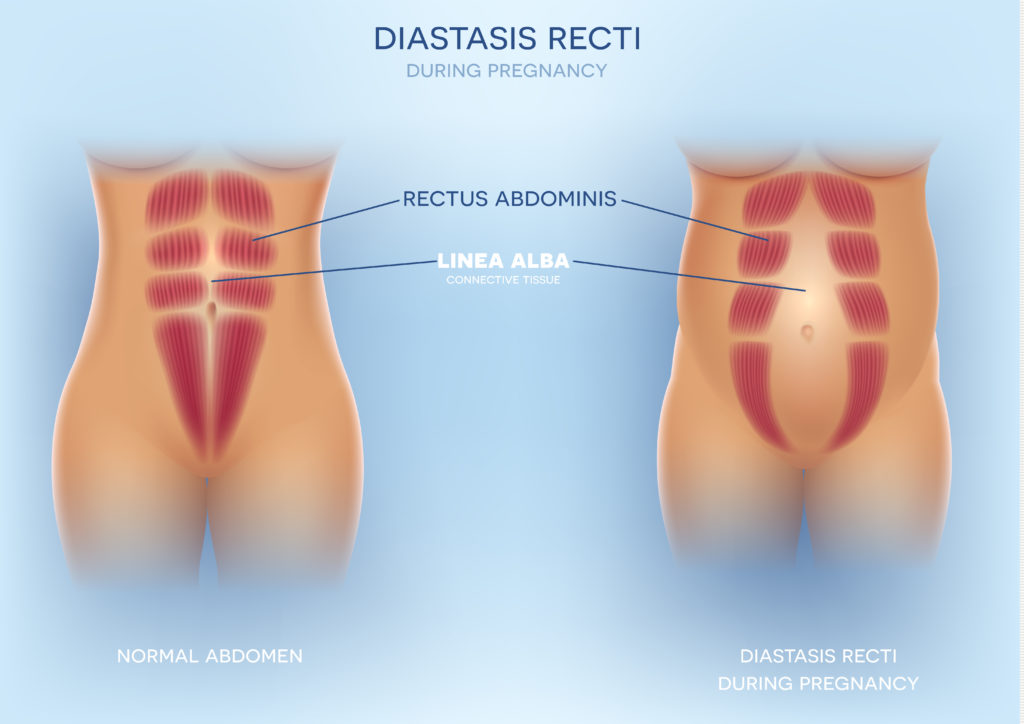
Diastasis Recti (DR), is classified as the separation between the left and right abdominal muscles which is commonly associated with pregnancy. DR is perfectly natural and it’ the body’s way of making space for your growing baby. In fact, a small study shows that 100% of women will have some degree of DR in the later stages of pregnancy (Mota et al 2014) and the abdominal muscles stretch for some women (Brauman 2008).
Within the first 8-weeks postpartum, the healing process will take place but for some women (like myself) the gap doesn’t completely close. But it isn’t about the gap and I’ll explain why in a bit.
Is DRA a problem?
Not usually. For most, it’s about building the core strength post-pregnancy. As your core gets stronger, your abdominal separation is generally a non-issue. As any healing process goes, it needs time and progressive overload. That’s it. Nothing fancy.
Just because you have a DRA, doesn’t mean you’ll automatically start peeing when you work out either like some fitness programs you find in Facebook ads suggest.
Antony Lo posted a study on his Instagram that looked at 300 women and found at 6 weeks postpartum, 15.9% of women without diastasis recti had a pelvic organ prolapse. (Bø et al 2017). This suggests women who did not have a separation within their rectus muscles, have a pelvic organ prolapse to some degree. However, it was originally thought there was a connection between abdominal separation and pelvic floor dysfunction which is why women needed to be concerned to begin with. The reason why is unknown at this point, but still pretty interesting.
If you’re concerned about DR, get assessed by someone with training and not a group on social media. If you find yourself feeling anxious about your DRA, see a pelvic floor PT. Spare your sanity and don’t go onto Facebook and ask in a mom group.
You can also do self-assessment to get an idea of what you’re working with. Click here to check out the video to learn how.
DR isn’t about the gap.
There are fitness and rehab programs which only focus on closing the gap when DRA isn’t about the gap at all. It’s about who your core works together as a unit. This unit made up of your diaphragm, pelvic floor, transverse abdominis, and multifidus.
If the core unit is all functioning well as a team and the Linea Alba is able to maintain tension, you don’t have to be concerned with the gap. ( Lee and Hodges Tension vs separation (Bø et al) debate)
Does having a DR mean that you have to cut out crunching or planking?
Depends. This isn’t a one size fits all. If you are able to maintain tension in your core as well as your Linea Alba, you’re good to go. The same goes if you see doming. Yes, if you have doming, and you’re able to maintain tension, you can do planks, crunches, overhead press, and hang from the ceiling.
On the other hand, if your core and Linea Alba feel squishy, you may not be ready. It doesn’t mean you have to omit those movements completely. Try various modifications, make sure you’re breathing and in neutral alignment, as well as adding in your kegel (if your pelvic floor physio says it’s ok to add in the kegel)
If you want your DR to heal, it needs to be challenged. Tissues get stronger when they are loaded. Avoiding exercise isn’t going to help in the long run.

In the past, it was thought if you had doming or coning during certain movements, it was best to modify or omit. However, if you’re able to maintain tension in your core and Linea Alba with the presence of doming or coning, it may be perfectly safe to continue. To be sure, you can book a free strategy call by clicking here.
DRA is a hot topic and it has women concerned about the long-term function of their bodies. But in most cases, your DRA doesn’t need much intervention unless there is a 2 or more cm separation. In that case, a pelvic floor PT or a coach with core and pelvic floor qualifications are the best training people to assist you. Want to train at a higher impact with a diastasis recti? I am currently accepting applications for Online Coaching. I only take 5 new clients at a time due to the intensive nature of this program. If you are ready to take on more but still feeling unsure about how to go about your training with your DR, click here to apply now. You will be contacted if you meet the qualifications.
Ciao for now,
Terrell
Ready to maximize your postpartum fitness performance? Get my
Resources:
- Relevance of open magnetic resonance imaging position (sitting and standing) to quantify pelvic organ prolapse in women.Abdulaziz M1, Kavanagh A2, Stothers L3, Macnab A2,3. https://www.ncbi.nlm.nih.gov/pubmed/29989885
- Positional pelvic organ prolapse (POP) evaluation using open, weight-bearing magnetic resonance imaging (MRI).Friedman B1, Stothers L2, Lazare D3, Macnab A2. https://www.ncbi.nlm.nih.gov/pubmed/26225170
- Pelvic floor muscle activity in different sitting postures in continent and incontinent women. Sapsford RR1, Richardson CA, Maher CF, Hodges PW. https://www.ncbi.nlm.nih.gov/pubmed/18760158
- Symptomatic pelvic organ prolapse and possible risk factors in a general population. Am J Obstet Gynecol. 2009 Feb;200(2):184.e1-7.


